Healing From Trauma; Addressing PTSD

Understanding PTSD is a HUGE part of healing from trauma. When we have intense, over the top reactions to seemingly random things, it can be extremely frustrating, especially when we don’t know why we’re reacting the way we are. This can cause a lot of anxiety and depression, in addition to avoidance of certain people and activities (isolation), which in turn can cause more anxiety and depression. PTSD has an incredibly negative impact on our lives. But knowledge is power! So get ready to learn some very helpful information!
In this article, we’re going to look at these elements of PTSD:
- Myths surrounding PTSD
- What are the symptoms of PTSD?
- What it is, what causes it? (yes, there is a real scientific, biological, medical explanation)
- What triggers it?
- How it feels when you’re triggered. (If you suffer from PTSD, you already know, but you might want to share this article with someone in order to educate them. Third party validation is sometimes needed for people to realize it’s a real thing!)
- How to help yourself when you’re triggered.
- How to help someone you love when they’re triggered.
Myth: Only soldiers who experienced combat suffer from PTSD
When my therapist told me I had PTSD (back in 2008) I felt guilty! I hadn’t been through the horrors my uncle had witnessed in Viet Nam that haunt him to this day! It didn’t seem right to say that’s what I was experiencing. I hadn’t “earned” it. That’s what many people, and possibly you, believe as well. But, while it’s true that some military personnel sadly develop PTSD after going through Hell and back, you’ll see, once it’s explained, that anyone who has experienced emotional, psychological or physical trauma, can suffer from PTSD.
Remember that emotional and psychological trauma is the result of extraordinarily stressful events that shatter your sense of security, making you feel helpless in a dangerous world. Psychological trauma can leave you struggling with upsetting emotions, memories, and anxiety that won’t go away. It can also leave you feeling numb, disconnected, and unable to trust other people.
While emotional trauma is a normal response to a disturbing event, it becomes PTSD when your nervous system gets “stuck” and you remain in psychological shock, unable to make sense of what happened or process your emotions. ~HelpGuide.org Read the whole article here: https://www.helpguide.org/articles/ptsd-trauma/coping-with-emotional-and-psychological-trauma.htm
What Are the Symptoms of PTSD?
If you think you might be suffering from PTSD but you’re not sure, perhaps looking at this list of common symptoms taken from activebeat.com will help.

- Physical Pain – headaches or migraines, dizziness, fatigue, chest pain, breathing problems and digestive issues. Chronic pain is a common sign!!
- Nightmares or Flashbacks
- Anxiety/Depression; irrational fears, avoidance of certain situations
- Withdrawal from social life, loss of interest in hobbies
- Avoidance of anything that might be a trigger
- Repression – intentional blocking of memories
- Emotional numbing; substance abuse
- Jumpy – easily startled; edgy, unable to ever relax for fear of possible threats
- Irritability due to the state of constant fear; sleep deprivation, inability to concentrate
- Guilt & Shame for not being able to regulate emotions
- Insomnia/Nightmares
- Fatigue
What IS PTSD? The Science Behind It
PTSD is an acronym for Post Traumatic (not post war) Stress Disorder. In essence, we’re traumatized at some point, and then suffer emotional flashbacks after the actual incident is over. We’ll talk about WHY that happens in just a moment.
Something very important to keep in mind is that occasionally we REACT to something, but can’t pinpoint what has triggered us, or even remember what caused the trauma in the first place. All we know is that we’re freaking out and can’t calm down (aka “emotional dysregulation”), and we feel like weirdos, or like we’re not normal, or that we’re going crazy. Being emotionally dysregulated can be REALLY distressing and lead us down a rabbit hole of negative thoughts. “Will I ever be normal?” etc..

In cases of extreme trauma, it’s common to suppress memories for years, even forever. Sometimes these memories start to resurface when we’re in an emotional state that’s stable enough for the mind to allow us to remember them (which seems counter-intuitive, because once you start remembering horrifying memories, you feel anything but emotionally stable).
Something helpful to keep in mind during these situations is that THESE ARE NORMAL REACTIONS TO ABNORMAL EVENTS. ~HelpGuide.org. You’re not broken. You’re not defective. The brain has incredible protective processes that come into action during and after traumatic events. Hopefully the explanation given by Tori Olds, below, will help you understand the science behind this. You’ll realize that you’re NOT weird, you’re NOT abnormal, and you’re NOT going crazy – even if you feel like you are. And as you keep reading, you’ll come to realize that there are things you can do to help yourself feel better.
Dr. Tori Olds

First, I cannot say enough good things about Dr. Tori Olds. She’s incredibly smart, and her information is organized, easy to understand, and immensely helpful. She has a very calming voice and disposition, and a kind face. Also, I think it’s ironic that her last name is Olds when she looks so young. 🙂 She has a video series on YouTube explaining IFS (Internal Family Systems) therapy. In one of the videos, “Healing Trauma in IFS Therapy,” she explains how the brain stores memories. I’ve never received IFS Therapy, but just listening to her explanations alone has helped me to realize why I act the ways I do. I’ll post a link to this video below.
She explains that during moments of extreme stress or trauma, the part of the brain that encodes memory is impaired, such that, when the trauma is recalled, it feels like it’s happening again. Those wounded parts of ourselves hold information around not only what we experienced, but how we felt at that time. Did I feel scared? Alone? Threatened?
“Most of the time when we remember our lived experiences, we understand that they happened in the past. However, our memories around traumatic or overwhelming experiences are stored differently in the brain. That’s because during moments of extreme stress, fear or trauma, our way of encoding memory changes. Why? Because stress hormones reduce the working of our hippocampus, and one of the hippocampus’s most important jobs is to take what’s happening, the thing we are coding into memory, and put a timestamp on it.”

She further explains that even though it “feels like yesterday” that she graduated from high school, she knows the difference between what really happened yesterday and something that happened 22 years ago. In the case of a traumatic memory in which the hippocampus did not put a timestamp, if something triggers that memory, it feels as though it’s happening NOW. We not only feel the exact same feelings we did at the time, we feel them as if we were the age at which they happened. This is called a flashback.
Honestly, I could go on a tangent with all of the information I’ve learned from this wonderful lady. But I’ll contain myself and just HIGHLY recommend that you look her up on YouTube and listen to the whole series. In later videos she explains that these traumatized parts do not define us, and that it’s possible to separate them from our other healthy parts in a process called Unblending.
Here is the link her the video I referred to earlier:
https://youtu.be/ThA1ojmekpI?si=6xI7-9PrUAMGzD-s
What Triggers PTSD
First of all, what is a trigger? A trigger is anything related to a traumatic event that reminds the person of what they experienced, and causes them to have a flashback.
Virtually ANYTHING can be a trigger. A scent, a sound, a word, someone who looks like someone else. A butterfly. A truck. A flower. Triggers may be unnoticed by most people and seem completely harmless. But to someone who suffered a traumatic event, it’s enough of a reminder to bring them back to that event and relive it.
How Does it Feel to Be Triggered, and How Long Does That Feeling Last?
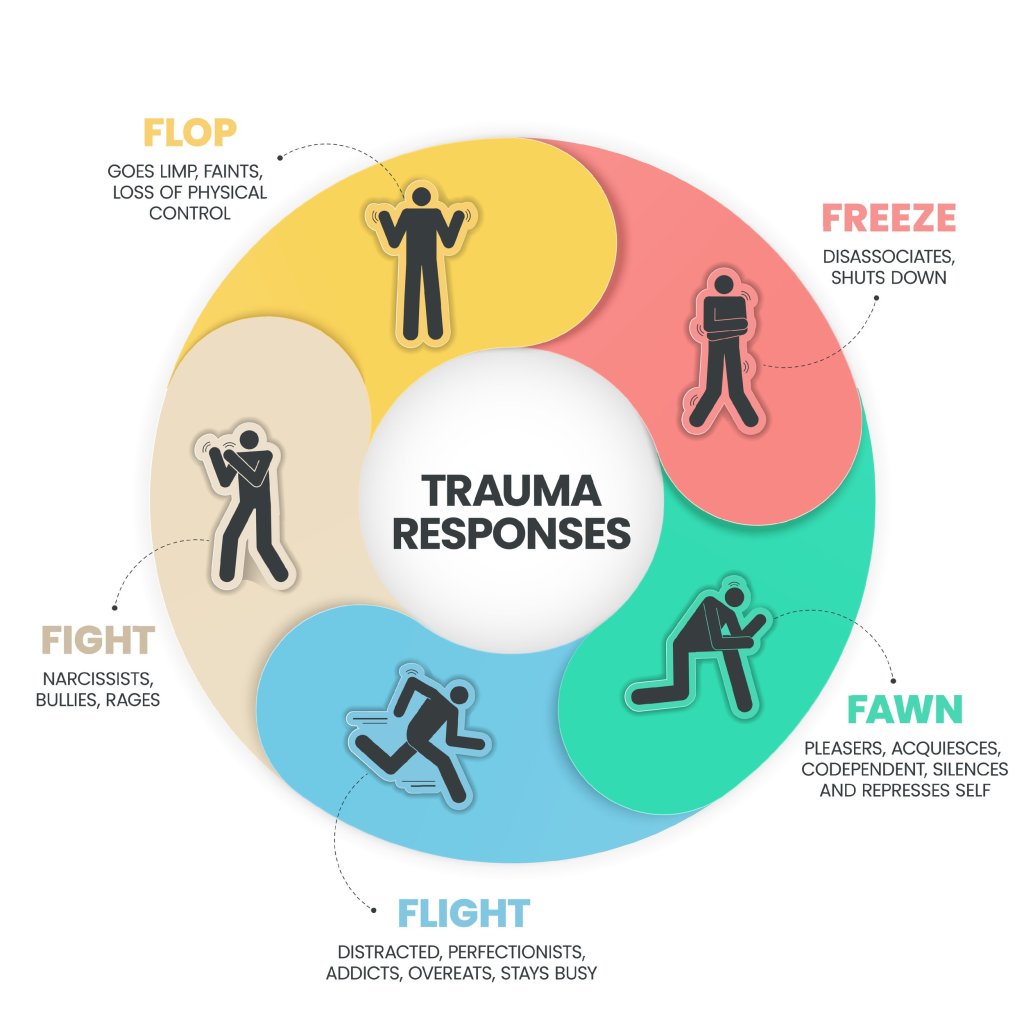
As stated before, when we are triggered, we experience emotional flashbacks, and we feel exactly the way we did when the event happened, and again, not through the lens of your current mature, evolved age at which you may have handled the situation differently. We feel as though we’re the exact age we were when the event occurred. Common responses are fight or flight, freeze or fawn. Even passing out. Whichever strategy your brain deems the most effective in keeping you safe at the time.
I can’t speak for everyone, but when I’m triggered, or even when I think I’m ABOUT to be triggered, I feel fear and terror equal to what I imagine I’d feel if someone were standing next to me with a gun to my head, or if I were standing on a tightrope 10 stories high without a net. It’s INTENSE. Physically, my heart begins to pound, my breathing gets shallow, I start shaking, and I have a sense that something horrible is about to happen. I want to totally freak out, run out of the room screaming, hide in a closet and never come out. But that’s socially unacceptable, so I sit quietly with all that pandemonium going on in my stomach, probably causing ulcers. Before he understood otherwise, my partner used to say, “You really handle your stress well.” I was too embarrassed to tell him how I really felt.
Triggers are instant and often unpredictable. They can happen in a millisecond, and sometimes aren’t even recognized. “Flashbacks happen when you relive some aspects of a traumatic event. It can sometimes be like watching a video of what happened, but flashbacks don’t necessarily involve seeing images, or reliving events from start to finish.” ~mind.org.uk These elements of PTSD are fast. The lingering part is the after shock – the feelings of terror, disgust, anger – that results from the trigger/flashback. Usually they are extremely intense in the beginning, and then dissipate over time. These negative feelings can last for days, weeks or even months. I have personally found that, as difficult as it is to do, being able to talk to someone regarding the incident and avoiding repeat triggers helps immensely. NOT talking about it only results in physical and emotional discomfort.
How to Prevent Triggers in the First Place
I actually deleted this paragraph, and then decided to put it back in. I took it out because there’s no answer to this question. The only way to really prevent triggers is to live in a bubble. If you suffer from PTSD, you know what I mean. There are triggers EVERYWHERE. Knowing this adds to our anxiety. We can avoid as much as we can, however, if we want to really live, we know that the risk of a trigger popping up out of nowhere is real. That’s why it’s vitally important to have strategies in place for when we’re triggered, AND to have an emotional support person or group.
That said, there are a few things we can do to temporarily avoid triggers. For example, I like to go out hiking. There’s nothing to trigger me during that activity. There’s the trail, rocks, dirt, trees, the sky, and me. It’s like giving myself a break from the world, and at the same time getting some fresh air and exercise.
How to Help Yourself When You’re Triggered
It’s very beneficial to plan some of these responses in advance so that you have some tools in your pocket when you’re unexpectedly triggered. I’ve been triggered unexpectedly, as you probably have, and it’s extremely difficult to regulate emotions and reactions in that circumstance.

Here are a few suggestions that I’ve found to be helpful:
- Remember that it’s a biological response to something that traumatized you
- Don’t feel bad that you’re reacting the way you are. Piling guilt and shame on yourself does nothing to help, and will only add to the negative feelings you’re experiencing.
- Remember that it’s not your fault!
- Something HAPPENED TO YOU. It’s not like you chose it.
- Breathe in slowly. Hold for five seconds. Breath out slowly. Repeat.
- Don’t underestimate the effectiveness of controlled breathing!!
- Ground yourself.
- Going outside, feeling the breeze, feeling the earth under your feet, will bring you back to the present moment.
- Look at your hands.
- See that they are not the hands of a child. This can also bring you back to the present moment.
- Have a support person or team.
- Share with your partner, as best you can, what happened in your past, and what triggers you. They can modify what they do or say around you, or be on the lookout for things that might trigger you and steer you away from them. This might seem to you like a lot to ask, but it probably won’t seem that way to the person who loves and cares about you.
- Share your plan with your person.
- Some people like to be held or touched when they’re triggered. For others, that’s the LAST thing they want.
- Have your partner take you outside and start asking you questions. That will take your mind off of what you’re focused on.
- Ask yourself what’s REAL, or what you REALLY know for sure.
- My friend was triggered by a list of girl’s names on her boyfriend’s fridge.. Because of her intense fear of abandonment due to a history of being cheated on, she believed it to be a list of potential replacements should she and her partner break up. She panicked, took the list, cut it up into a million pieces, and threw it in the trash.. In the end, she learned it was a list of dog sitters.
How to Help Someone When They’re Triggered
Being around someone with PTSD takes a lot of patience. Above all else, validate their feelings. Let them know that you understand that PTSD is real, and that you’re there to support them.

It’s hard to know what might trigger your loved one, so it will take time to become familiar with those smells, sounds, and sights. They might not even know all of the things that could be potential triggers, and the pressure of trying to identify them can cause a lot of stress. It can also be embarrassing to share these things, so again, patience is key.
If it’s a romantic partner that has PTSD, you have some decisions to make. Are you ok with avoiding the things that trigger them? Are you ok with modifying what you say and do around them? Are you willing to help shield your partner, or alert them of potential triggers? And are you willing to do what it takes to help them in the event that they are triggered?
It’s hard to witness someone you care about experiencing intense fear and anxiety, and not completely understanding why. It might feel as though you’re walking on eggshells around them, watching everything you say and do so as not to trigger them. This can get tiring. You may need a support system yourself, a friend to vent to now and then.
Let me state here for the record that I DO NOT believe it’s anyone’s responsibility to change for another person unless the person doing the changing is willing and able to do it. I also believe it’s a two way street! I’ve said to my partner that I certainly don’t want him to change who he is because of my issues. He tells me I’m making him a better person because of the things I ask him to avoid saying, doing and watching. At the same time, I’m seeking therapy so that I can learn ways to better react to my triggers. It definitely takes teamwork!
Things that help & things that don’t.

- Limiting stressors: Limiting stressors WILL NOT eliminate Emotional Flashbacks, but it will certainly help with the amount, duration, and intensity of them. This is why. Picture a drinking glass. If you pour into the glass works stress, relationship stress, stress from taking care of children, maybe your car breaks down. Your glass is getting pretty full. Then comes along a Trigger. You dump that into the glass, and the glass cannot handle the amount of emotion you’ve poured into it, and it overflows. This looks like varying degrees of crying, anxiety, irritation or an all out emotional meltdown.
- Being selective in what we choose to engage in.
- We can avoid or eliminate activities surrounding known triggers.
- We can reduce some of the things that make us feel pressured
- We can counteract stressful situations with activities such as meditation, exercise, reading, journaling, yoga, singing, zumba – whatever helps you decompress.
Just a quick word about meditation. Personally I have trouble sitting still trying to clear my mind. My brain never stops. So, here are some meditation strategies that have worked for me.
- Mowing the yard. The constant sound of the mower relaxes me. Also, I have to focus on what I’m doing, but it’s not so technical that inspired thoughts don’t enter my mind. My best ideas and moments of greatest creativity usually happen when I’m mowing the lawn.
- Identifying bird sounds. It may sound silly, but when I sit outside, I focus on all of the bird sounds I hear and try to identify them. It takes my mind off of what’s causing me to be anxious.
Treatment: Medication and Therapy
Medication: Because I am neither a licensed psychiatrist, psychologist, or medical doctor, I don’t feel comfortable advising in this area. Also, I don’t have much personal experience with medications for PTSD, anxiety and depression. Information on the internet says that doctors most often prescribe SSRIs or SNRIs. Both treat anxiety and depression.
I’m not ashamed to share that I have recently started taking an SSRI due to the level of anxiety and depression I’ve been experiencing recently due to life changes (my best friend just passed away in July. I moved to CO from FL, so new job, new friends, new everything.. My children all live very far away now; one in Scotland, one in Maui, one in Tampa, FL.. I’m in a new relationship which definitely stirs its own bees nest of triggers and flashbacks.) I’ll let you know how it goes!
Therapy

In addition to, and possibly more important than medication, is therapy! We are not equipped to deal with some of the things we’ve been through. There is no shame in talking to someone and getting advice from someone who has studied the workings of the brain! When we want to know how to do anything better, what do we do? We talk to experts in that area! This is no different.
I truly believe that in recent years we’ve learned so much about how trauma affects the brain. Trauma literally shapes how our brains function and process! The good news is that our brains are neuroplastic, meaning they have the ability to be rewired, and to function in some way that differs from how they previously functioned. There are new methods of therapy available today that we didn’t have years ago.
If you Google “Best Therapies for PTSD” you’ll come up with this list. I’ll briefly explain each, and put my own comments in parentheses
Strongly Recommended on Google
- Cognitive Behavioral Therapy (CBT) » …
- Negative patterns of thought about the self and the world are challenged in order to alter unwanted behavior patterns or treat mood disorders such as depression
- Cognitive Processing Therapy (CPT) » …
- A specific type of CBT. 12 sessions.. You’re taught how to evaluate and change the upsetting thoughts you have had since your trauma. By changing your thoughts, you can change how you feel
- Prolonged Exposure » …
- (By name, this sounds like Hell to me). It’s a form of CBT in which there are two main treatment procedures.
- Imaginal exposure – intentional repeated retelling of your trauma and gradually confronting situations, places, and things that are reminders of the trauma, or feel dangerous (in spite of being objectively safe)
- (By name, this sounds like Hell to me). It’s a form of CBT in which there are two main treatment procedures.
- Eye Movement Desensitization and Reprocessing (EMDR) Therapy » …
- Apparently this type of treatment is controversial. It’s purpose is to alleviate distress associated with traumatic memories such as PTSD
- I’ve heard a LOT of good things about EMDR from friends. They’ve said that it’s important to include the sensory elements – either tapping or buzzers.
- Narrative Exposure Therapy (NET) » …
- Used mostly with individuals suffering from complex and multiple trauma. It’s used most often in group or community settings and with individuals who experienced trauma as a result of political, cultural, or social forces, such as refugees
Not listed by Google: (probably because they are relatively new):
- Accelerated Resolution Therapy (ART):
- The goal is to help the individual reprocess traumatic memories and experiences in a way that reduces distress and promotes healing.
- The therapist guides the client through a structured process that involves visual imagery and rapid eye movement.
- (I have gone to a few sessions. My therapist was lovely. The therapy did not work for me. I believe it might be because my trauma is multi-faceted and has spanned decades).
- Internal Family Systems (IFS)
- Developed by Richard C Schwartz in the 1980s, IFS takes the view that our brains are made up of “relatively discrete subpersonalities, each with its own unique viewpoint and qualities.” ~Wikepedia
- As I mentioned above, Dr. Tori Olds is an expert in this area. I have never received this treatment, however just listening to her explanations of how the brain processes trauma has been immensely helpful. I HIGHLY recommend listening to her YouTube Videos.
- Talk Therapy
- Let’s not forget about good old Talk Therapy! Sometimes your trauma is too much for your friends to hear – it’s upsetting. Or you may need to talk about it more than they’re willing or able to listen. This is when talk therapy is a good idea.
- It’s nice to have a third party, someone who doesn’t know you, someone unbiased, to listen and offer their expertise and validation.
Regardless of what type of therapy you choose, finding a good fit is essential. You have to feel comfortable with the person you’re going to share intimate information with. Most therapists will offer a free 15 minute consultation. That’s usually enough to help you decide whether or not you want to make an appointment.
In Summary
PTSD is Post Traumatic Stress Disorder. Anyone who has experienced trauma can suffer from it. Triggers remind us of the trauma we experienced and cause flashbacks in which we feel as if the traumatic experience is happening presently. This phenomenon is due to the suppressed function of the hippocampus (the part of the brain responsible for putting timestamps on occurrences) due to excessive stress and overwhelm. PTSD is not your fault. It is a real thing. Knowing that there is a scientific explanation for severe reactions to triggers can be helpful. There are ways to lessen the negative emotions related to it. Having a support person or group is essential. There are many good therapies and medications that can also help. Please seek the advice of a professional before starting any therapy or medication.
As always, I hope you benefited from reading this article. This blog is my passion project. I write when I’m inspired by my own life events or those of others I’m close to. I share in hopes of helping others. Never forget that you are important, you are loved, and you are here on purpose!
If you feel so inclined, feel free to read some of my other articles below!
~Cheryl
-
My Story & My Mission
-
Narcissists Make You Sick. Literally!
-
The Grip of the Narcissist; Do We Want to Be Freed?
-
Narcissist Partners & Why We Stay: Cognitive Dissonance.
Leave a comment